Paying you for your services
What and how we pay you depends on the services you provide and the contract, legislation, or agreement you're working under.
On this page
When we’ll pay for your services
We'll pay you for treating a client’s injury as long as it’s:
- the most suitable option for their condition
- of acceptable quality
- given at the right time and place, with only the necessary number of treatments needed
- given by a provider with appropriate qualifications and a current annual practicing certificate
- clearly documented
- pre-approved by us, if pre-approval is needed.
When we decide what we’ll pay for, we also look at:
- the type of injury and its severity
- if it's a generally accepted form of treatment in New Zealand
- other options available in New Zealand to treat the injury
- the cost and benefit to the client of each treatment option.
How we’ll pay for your services
You can work with us in three different ways. How, and how much we’ll pay for your services depends on how you work with us.
If you work under the Cost of Treatment Regulations
The Cost of Treatment Regulations set out:
- who we'll pay
- how much we'll contribute to the cost of treatment
- the types of treatment we'll pay for.
Liability to Pay or Contribute to Cost of Treatment Regulations 2003
Working Together – A handbook for Cost of Treatment Regulations providers
If you work under contract
Your contract will set out the:
- service we're purchasing
- amount we'll pay for the service
- how to invoice us electronically.
If we ask for your services by purchase order
We may ask you to provide a service that's not included in Regulations or a contract, for example, client accommodation. In this case, we'll send you a purchase order that includes the:
- purchase order number
- type of service and the service item code
- date range we’ll need the service
- amount of the service we need
- amount we'll pay you.
How much we'll pay under the Cost of Treatment Regulations
How much we can pay towards your treatment services depends on:
- the type of services you provide
- if it includes procedures
- the type of provider you are.
General practitioners, nurses, and nurse practitioners
If you're a general practitioner, nurse, or nurse practitioner, we can contribute to two parts of your treatment services:
1. A consultation rate – including joint consultations
We pay a higher rate for clients under 14 years, and community services cardholders and their dependants (14 to 17 years) to compensate you for providing them with free visits.
Sometimes both a nurse and a general or nurse practitioner treat a patient during the same visit. If they make relevant patient notes, we'll contribute to both of these through a joint consultation rate.
2. Specific treatments or procedures a patient might get during a visit
We'll only contribute to the cost of the treatment or procedures set out in the Regulations.
General practitioner, nurse and nurse practitioner costs, from 1 June 2024 (ACC1520)
Changes from 1 June 2024
Cost of Treatment Regulations pricing to increase 1 June 2024
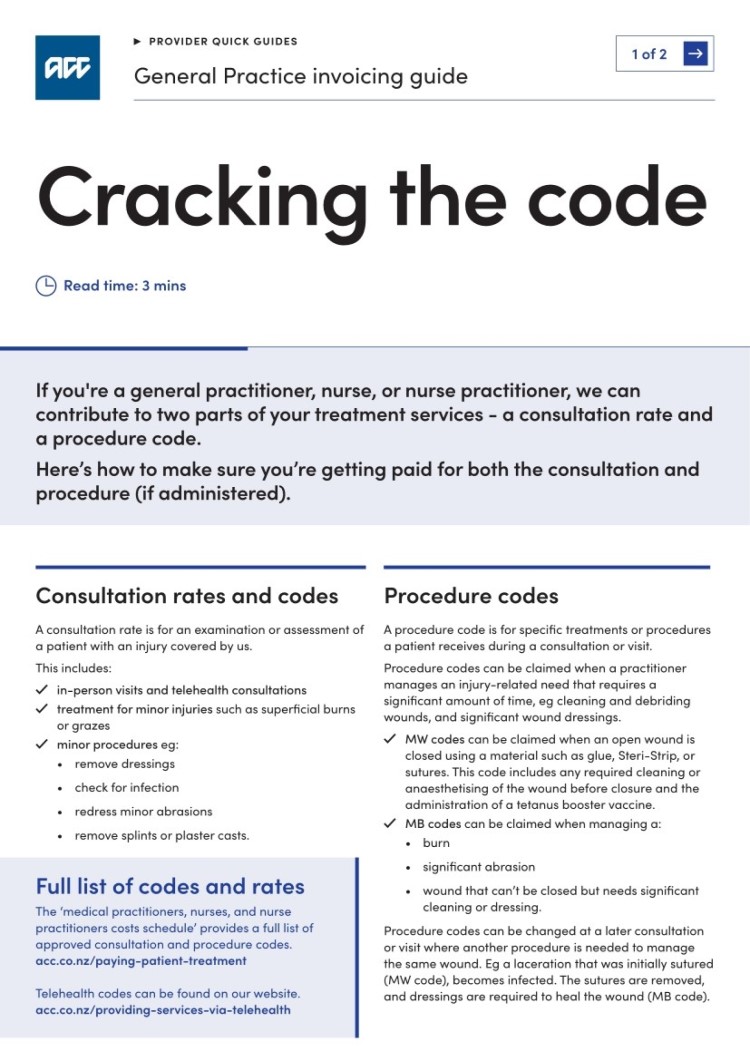
Quick guide: General practice invoicing
If you're a general practitioner, nurse, or nurse practitioner and are invoicing us under Cost of Treatment Regulations, we can contribute to two parts of your treatment services - a consultation rate and a procedure code. Here’s how to make sure you’re invoicing for both the consultation and procedure, if administered.
Medical specialists
If you're a medical practitioner who practices in one or more of the recognised branches of medicine, we'll pay the amount set out in the Regulations.
Registered specialist costs, from 1 June 2024 (ACC1519)
Specified treatment providers
Specified treatment providers include:
- acupuncturists
- chiropractors
- occupational therapists
- osteopaths
- physiotherapists
- podiatrists
- speech-language therapists.
As a specified treatment provider, you can choose to be paid by time or per treatment.
Specified treatment provider costs, from 1 June 2024 (ACC1523)
Time-based
If you're invoicing us for time-based treatment, we'll pay for the time you spend completing direct treatment on your client. It should be rounded to the nearest five-minute increment.
For example, if you provide direct treatment for 43 minutes, this can be billed as 45 minutes of treatment to ACC. If you provide direct treatment for 37 minutes, this should be billed as 35 minutes.
You can't invoice us for more than 60 minutes in any hour that you're treating our clients. For example, if you see three patients in an hour and spend 20 minutes with each client, we expect to see invoicing for three clients at 20 minutes each.
Paid per treatment
This is a fixed rate per treatment. If you're treating a patient with more than one injury, you can't combine the number of treatments of the different injuries.
If the client needs more treatment for those injuries, you'll need to get pre-approval.
Getting pre-approval for patient treatment
Same-day treatment
We generally only pay for one treatment from one specified treatment provider per client per day. We may pay for more than one treatment from a specified treatment provider(s) per client, per day if this meets our legislative requirements and is also clinically justified.
Multiple same-day treatment position statement
Audiologists
If you provide hearing loss services, we have a guide for providers working under the hearing loss regulations. It includes how much we'll contribute to heading aids and other hearing services.
Hearing loss services, from 1 June 2024 (ACC8043)
Counsellors
If you're a counsellor, or a counsellor who's a medical practitioner, we'll pay you a fixed hourly rate set out in the Regulations.
Counsellor costs, from 1 June 2024 (CTRIS02)
Dentists
If you provide dental services, we can pay for a client's consultation and treatment. How much we pay is set out in the Regulations.
Dentist costs, from 1 June 2024 (ACC1522)
Radiologists
If you're a radiologist, we'll pay at a fixed rate for imaging services and treatments or procedures. How much we pay is set out in the Regulations.
High-tech imaging services are only paid under contract.
Radiologists' costs, from 1 June 2024 (ACC1521)
Optometrists
If you’re an optometrist, you will need to bill us using the correct codes which are a flat fee for consultations. Please note some codes require prior approval.
ACC8440 Optometry Codes from 10 October 2022
Telehealth Services
If you are eligible to provide telehealth services, we’ll pay you the rates set out in the regulations.
Telehealth service codes and rates, from 1 June 2024
How we fund providers in training
We only pay for treatment given by qualified providers.
If you're a provider in training, eg an intern or a university or polytechnic student undertaking practical work for study, we can offer to fund you if you're:
- already a qualified practitioner undertaking further study
- unqualified but have gained consent from the patient and are supervised by a qualified practitioner who:
- is present throughout the treatment delivery
- takes responsibility for assuring treatment is up to standard.
Position statement - Seeking payment for treatment by allied health students
Paying for lodging a treatment injury claim
We can pay towards the administrative costs of lodging a treatment injury claim, for example, recovering medical records. We'll pay you as long as all of the claim forms are completed, even if we deny the claim.
The costs of lodging a treatment injury claim is separate from payments we make towards the costs of consultation and treatment.
| Type of provider lodging the claim | Forms you need to include | Straight forward or moderate claims | Complex claims |
| District Health Board |
|
$40.00 | Your hourly rate |
| Private hospital |
|
$40.00 | Your hourly rate |
| Other health professional |
|
$24.00 | Your hourly rate |
Invoice us for this separately from treatment costs:
How we'll pay pharmaceutical costs
We pay for prescribed medications:
- by contract - if the contract includes providing medications, patients shouldn’t be charged any costs for prescribed pharmaceuticals
- via Public Health Acute Services (PHAS) bulk payment that we pay to the Crown. This covers pharmaceuticals that are:
-
- required by clients during acute hospital admissions or emergency department visits
- given as part of the treatment associated with clients’ outpatient follow-ups for up to six weeks from discharge or treatment
- used during treatment given by medical practitioners less than seven days after referrals by other medical practitioners
- listed on the Pharmaceutical Schedule, meet its subsidy criteria and are used in the community.
If prior-approved, we reimburse clients or pay pharmacies:
- for co-payments on community pharmaceuticals
- a contribution towards part-charges for partly subsidised pharmaceuticals or pharmaceuticals that aren’t on the Pharmaceutical Schedule.
When assessing funding requests, we’ll look at:
- best practice prescribing protocols
- rehabilitation pathways
- generic alternatives listed in the Pharmaceutical Schedule
- the approved use of the medicine in New Zealand.
If there isn’t enough information to support the request, we may ask you for more information.
Pharmaceutical costs we don't cover
We don’t cover:
- any administration charges added by you or the dispensing pharmacy
- the cost of substances not considered pharmaceuticals, such as herbal remedies and complementary medications.
When to seek prior approval for pharmaceuticals
If your client needs long-term pharmaceuticals or non-subsidised pharmaceuticals not already covered by the PHAS time period or under another contract, you’ll need to seek funding approval from us by completing the ACC1171 Request for pharmaceutical funding form before prescribing the medicine. This will help to tell us why the pharmaceutical is needed for injury management.
Contact us
If you have any questions, contact us:
Phone 0800 222 070 (Monday to Friday, 8am to 6pm)
Email providerhelp@acc.co.nz